On Tuesday, August 15, the Centers for Medicare and Medicaid (CMS) published a proposed rule to reverse many of the policies surrounding bundled payments that had been initiated under the Obama administration. The Secretary of Health and Human Services (HHS) Tom Price had voiced his opposition to bundled payments before assuming his current role in the Trump administration, and therefore this move does not come as a great surprise. In fact, you may recall we discussed the potential for a policy reversal on bundled payments in a blog post in January, predicting that the Comprehensive Care for Joint Replacement program (CJR) would shift from a mandatory program to a voluntary one. While the new proposal from CMS does not eliminate mandatory bundles outright, the fact that Secretary Price is directing CMS to draft regulations that reflect his view of bundled payments was not unexpected.
The proposed rule offers two points of action: first, reduce the number of hospitals in which CJR is required and second, eliminate new bundled payment programs. CJR is a required bundled payment program in 67 markets throughout the U.S. The proposal aims to shrink that number to 34; the remaining 33 markets can participate voluntarily, and some low-volume and rural hospitals located in the remaining 34 markets will also be exempt from mandatory participation. Currently, Medicare pays a lump sum dollar amount for patients undergoing joint-replacement surgery in these 67 markets. The lump sum is designed to cover both acute and post-acute care needs. In theory, physicians may be encouraged to send recovering patients home with home health and physical therapy or simply home with outpatient physical therapy to maximize their profit because those post-acute care options typically cost considerably less than a short-term stay in a skilled nursing facility. One potential result of removing the mandatory bundled payment arrangement may be to encourage physicians to refer patients to skilled nursing properties once again and thereby potentially increase the Medicare census for those skilled nursing properties located in the 34 markets that would no longer be required to participate in the program.
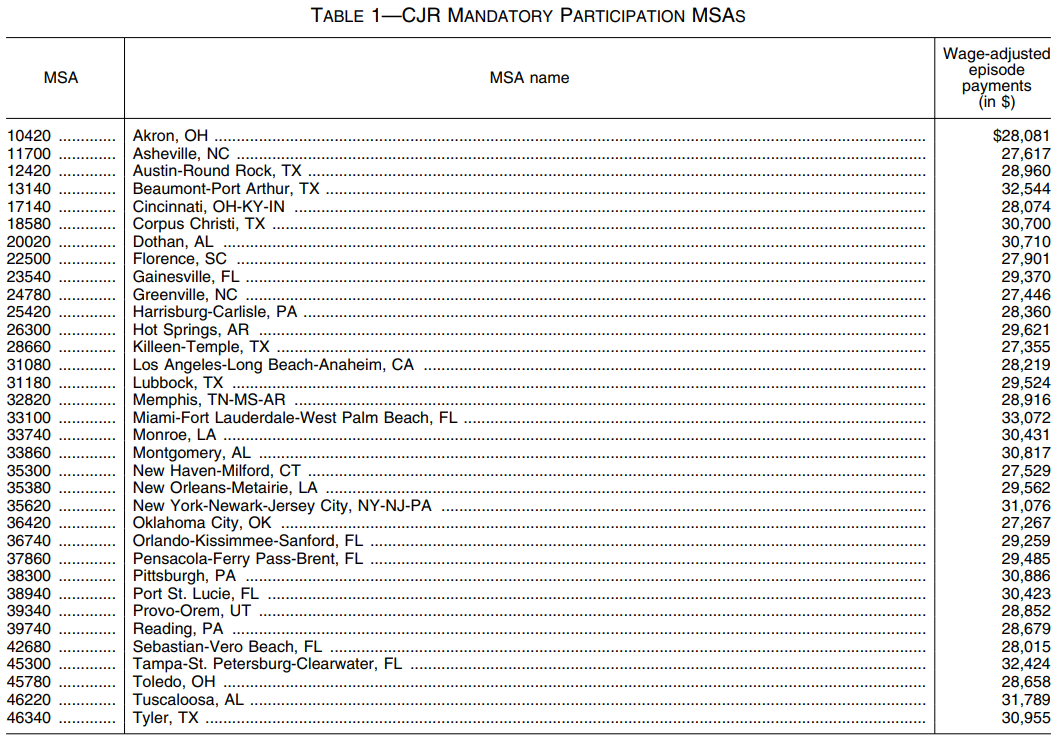
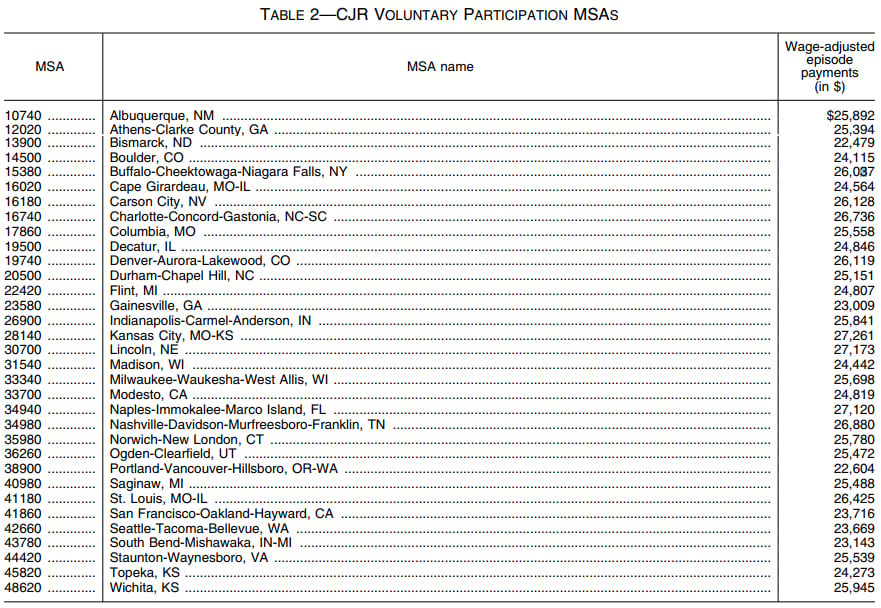
Source: Federal Register Proposed Rule: Medicare Program; Cancellation of Advancing Care Coordination Through Episode Payment and Cardiac Rehabilitation Incentive Payment Models; Changes to Comprehensive Care for Joint Replacement Payment Model (CMS-5524-P)
The second proposed action in the rule eliminates new bundled payment programs that operate like CJR but are applied to patients treated for cardiac episodes and certain fractures (read more about these bundles in the NIC Insider here). The new bundles had already been postponed under Secretary Price; in fact, the delay was one his first actions as HHS Secretary. Because these bundles had not yet taken effect, the prospect of removing them should not have an immediate impact on skilled nursing census. Skilled nursing providers who were anticipating a reduction in Medicare census following implementation of these additional bundles may need to reconsider. The predicted impact of the cardiac and fracture bundles on Medicare census may have already been less significant than CJR, as the patients in the new bundle programs would generally be higher acuity and therefore less likely to be eligible for less expensive post-acute options that undercut skilled nursing market share for CJR patients.
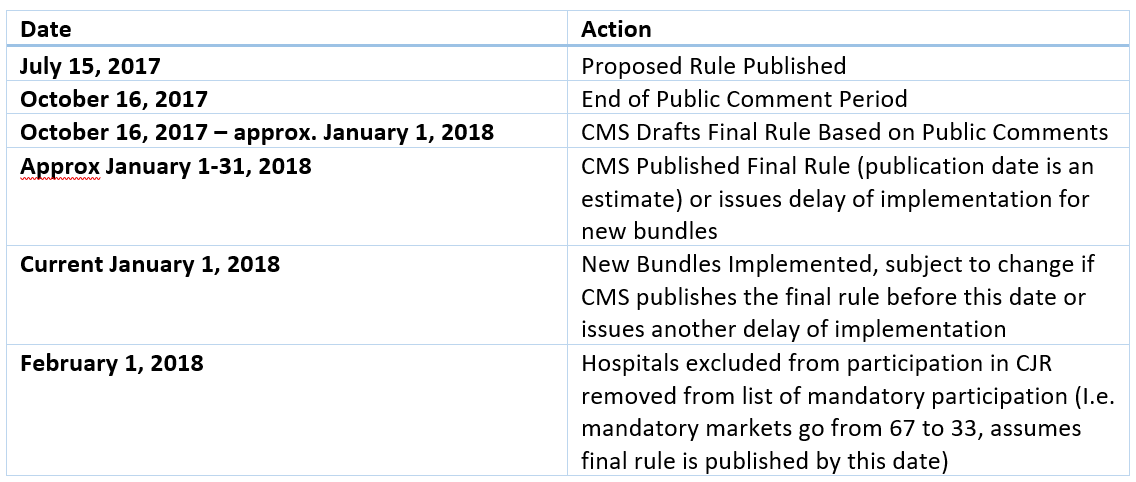
The proposed rule was published Tuesday and is open for comments from the public until October 16. CMS will then consider the comments and publish a final rule, so the end product may be different from this proposed rule. The final rule could be published before the implementation date for the new bundled payments which was scheduled for January 1, 2018, but CMS will probably need more time to process the comments and draft the final rule. Nonetheless, the new bundles will not likely take effect in January as CMS will either have published a final rule eliminating them or issued another delay in implementation to provide the agency more time for evaluation. The proposed rule uses February 1, 2018 as the date for which eligible hospitals transition from mandatory to voluntary participation, so CMS will likely do all it can to publish the final rule before that date. We will be keeping track of this policy development as it unfolds.
Look for more discussion on this exciting and evolving topic discussed at the upcoming 2017 NIC Fall Conference, September 26-28 in Chicago!
About Liz Liberman
Healthcare Analyst Liz Liberman provides policy, regulatory, and healthcare perspective to the dynamic environment surrounding the seniors housing and care market. She comes to NIC from the Department of Defense, where she served as a contractor in Acquisition policy, implementing statutes, executive orders, and updates into the Federal Acquisition Regulation (FAR) and Defense Federal Acquisition Regulation Supplement (DFARS). She also served as a health policy analyst for Bulletin Intelligence, where she crafted daily briefings for government agencies and trade associations in the healthcare field. Liz earned degrees from The George Washington University (B.S.) and George Mason University (M.S.), and is a member of the Junior League of Washington.
Connect with Liz Liberman
Read More by Liz Liberman