The primary tool the Centers for Medicare & Medicaid Services (CMS) has for enforcing care standards at skilled nursing properties are civil monetary penalties (CMPs). CMPs are essentially fines for facilities found to be out of compliance with CMS care standards. Based on a national average, CMS penalties for skilled nursing properties had been on the rise from 2016 to the third quarter of 2019.
Impact of the COVID-19 Public Health Emergency
As the country began to grapple with the COVID-19 pandemic and the public health emergency was announced, average CMS penalties for skilled nursing properties declined. This is likely a reflection of the more collaborative, less-punitive surveys that took place while surveyors – the CMS regulatory staff who assess compliance with Medicare health and safety regulations – and operators alike learned about COVID-19 and its spread.
A new federal government administration and a more thorough understanding of COVID-19 and the importance of strong infection control measures may mean that these penalties could be on the rise again, a trend that seemingly has already begun.
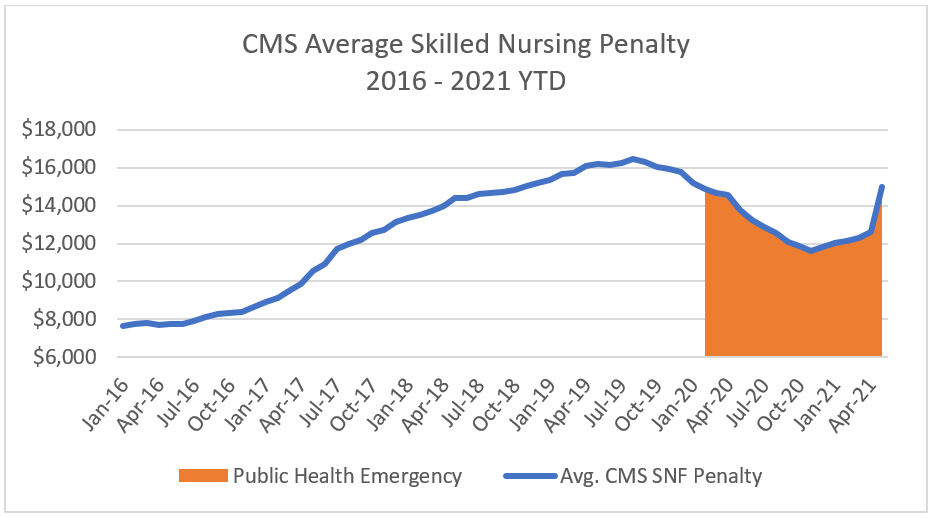
Source: Data.cms.gov; Nursing Home Services Data Archive, 2016-2021
A Rise in Per-Incident Penalties
Skilled nursing properties can be penalized through the imposition of a CMP for either the number of days that a facility has been out of compliance with a federal requirement (per-day or per-diem), for each instance of noncompliance (per-instance), or CMS can deny payments for new admissions. In 2017, guidelines were changed to set per-instance CMPs, rather than per-day, as the default penalty. Per-day penalties are often applied retrospectively and can accumulate to significant fines. Although per-day penalties remained the recommended approach for major violations, their overall use has been curtailed substantially.
This transition has meant that the total amount of fines collected through per-incident penalties increased more than eight-fold from 2016 to 2020 and are projected to be even higher at the completion of the 2021 fiscal year (on September 30, 2021). As per-day penalties can be applied retrospectively and accumulate to significant amounts, operators benefitted during these years, as they were sheltered from penalties above the per-incident maximum fine of $20,965. There is no cap on the accumulation of per-day penalties. The Center for Medicare Advocacy has opposed the switch to per-incident fines and has been working to reverse what it considers to be efforts to roll back skilled nursing resident protections.
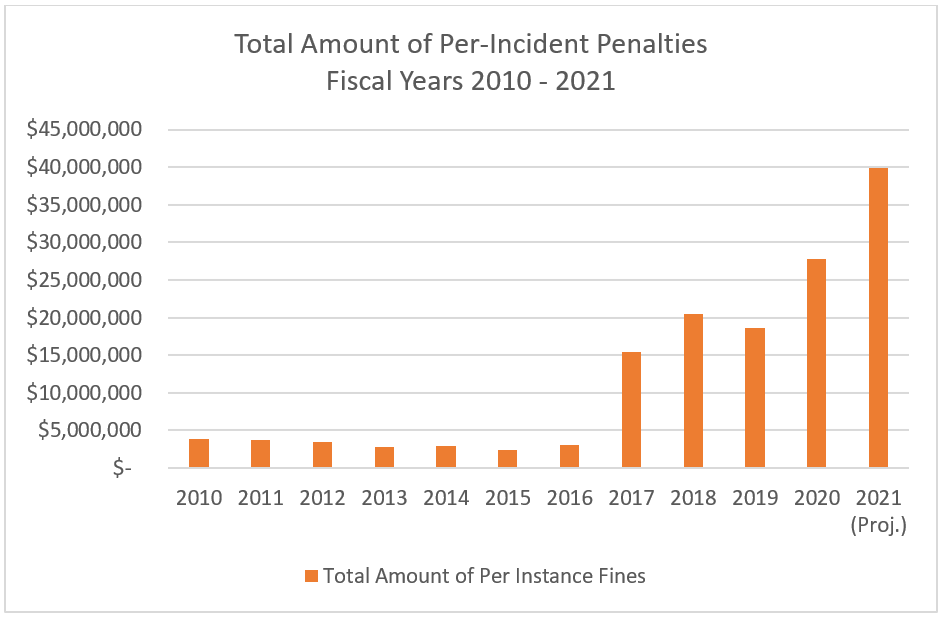 Source: CMS Quality, Certification, & Oversight (QCOR) Reports
Source: CMS Quality, Certification, & Oversight (QCOR) Reports
At the time of the policy change, Dr. Kate Goodrich, director of clinical standards and quality at CMS, said in a statement that unnecessary regulation was the main concern that health care providers raised with officials. “Rather than spending quality time with their patients, the providers are spending time complying with regulations that get in the way of caring for their patients and doesn’t increase the quality of care they provide,” Dr. Goodrich said.
With a new federal administration, high vaccination rates among skilled nursing residents, and the U.S. Senate confirmation of CMS Administrator Chiquita Brooks-LaSure, we could see a change in focus and policy and possibly a return to a stricter, and potentially costlier, enforcement.
CMP’s Impact on Workforce and Labor
Under current law, skilled nursing properties that are assessed civil monetary penalties above a certain threshold on their annual survey automatically lose their authority to train staff to be Certified Nursing Assistants (CNAs) for two years. With critical shortages in labor pools routinely being reported, particularly among CNAs, this penalty could have a major impact on a skilled nursing property’s staffing pipeline.
In February 2019, the bi-partisan Nursing Home Workforce Quality Act was introduced, which would allow suspensions on in-house CNA education to be rescinded once the related deficiencies are remedied, albeit while allowing additional oversight of skilled nursing properties. The Nursing Home Workforce Quality Act did not receive a vote from the 119th Congress, and in-house CNA training programs can still be impacted by a certain level of civil monetary penalties, even if the fines are unrelated to the quality of care given to residents or if the care deficiencies cited on the survey are unrelated to the CNA training program.
While penalties from CMS are an essential tool for ensuring skilled nursing properties are complying with care standards and are protecting their residents, both the approach and severity can be markedly different between administrations. A greater emphasis on infection control has broadened the scope of surveys, and subsequently the amount of time and resources involved in survey preparation. Without additional funding, a revival of more stringent surveys and quality standards could result in added annual costs for operators.
About Ryan Brooks
Senior Principal Ryan Brooks works with the research team in providing research, analysis, and contributions in the areas of healthcare collaboration and partnerships, telemedicine implementation, EHR optimization, and value-based care transition. Prior to joining NIC, he served as Clinical Administrator for multiple service lines within the Johns Hopkins Health System, where he focused on patient throughput strategies, regulatory compliance, and lean deployment throughout the organization. Brooks received his Bachelor’s in Health Services Administration from James Madison University and his Master’s in Business Administration from the University of Maryland.
Connect with Ryan Brooks
Read More by Ryan Brooks