Mental health is part of physical health. If that wasn’t always obvious, it became painfully apparent during the pandemic. Isolation and loneliness can trigger anxiety and depression.
Senior living residents can be especially vulnerable. Many residents move in with chronic health conditions, such as congestive heart failure, which can be addressed. Less recognized is the fact that mental health issues are also common among the older population.
But that’s changing. Awareness is growing among owners and operators that residents’ mental health issues need to be addressed. “Mental health challenges are being talked about more routinely these days,” said NIC Senior Principal Ryan Brooks. “That’s a good thing.”
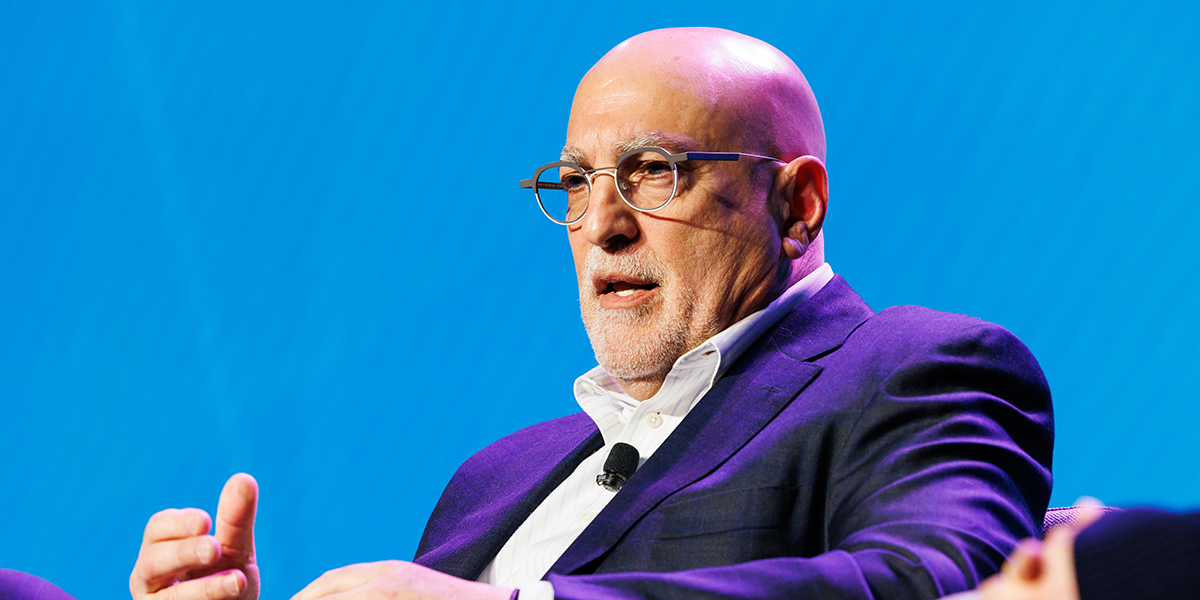
Brooks led a panel of experts at the 2023 NIC Spring Conference in a discussion titled, “Opportunities in Behavioral Health.”
The speakers addressed how owners and operators are integrating mental health programs into their offerings. The panel also discussed how some senior living providers are exploring whether underutilized properties could be recycled as behavioral health centers.

By the Numbers
A recent study by NORC, the research arm at the University of Chicago, conducted through a grant from NIC, found that more than half of senior housing residents have at least one mental or behavioral health diagnosis. Four out of five nursing home residents have a behavioral health diagnosis.
AARP found that 35% of older adults are lonely and prone to depression, leading to a higher risk of problems with alcohol and substance abuse. Twenty percent of seniors already suffer from some form of substance abuse, according to the Substance Abuse and Mental Health Services Administration.
“Positive health outcomes are not just nice to have,” said Brooks. Poor mental health can impact the resident’s ability to engage with their provider, keep appointments and take their medications.
Compromised mental health also hinders social engagement, according to panelist Hilary Forman, chief clinical strategies officer at HealthPro Heritage, an integrated health and wellness company that helps communities implement therapy, wellness and life enrichment programs. “We should be able to openly talk about this,” she said.

Beyond Awareness
A shift is needed from simple awareness of the problem to the establishment of clearly defined protocols and services, said panelist Richard Feldman, co-founder & managing principal, Behavioral Health Advisory Group. He added that the growth of telehealth is a step in the right direction, especially to supplement the shortage of mental health specialists.
Brooks asked about the role of the staff at the community. The first step is to train the staff about the importance of mental health. They should be aware of any diagnoses in the resident’s electronic medical record.
The staff should look for red flags. How does the resident behave? Is the resident attending programming? Going to dinner? “Look for simple clues that indicate isolation or a change in behavior,” said Forman. Also, big life events such as the recent loss of a spouse followed by a move to a community often puts a new resident at increased risk.
As a start, Feldman conducts an educational needs assessment with the entire staff. That forms the basis of protocols, such as when the CNAs should report a behavior or incident to a nurse who might need to report that to a physician. The goal is to integrate a behavioral health framework into resident programming and staff training. “I think you begin there,” he said.
The Real Estate Play
Some senior housing owners and operators are expanding their portfolios with dedicated mental health facilities. Substance abuse treatment centers and short-term psychiatric hospitals represent an opportunity for the industry, according to panelist Talya Nevo-Hacohen, chief investment officer at Sabra Health Care REIT. She said the trend is being driven primarily by insurance companies willing to pay for treatment.
Sabra has had some success recycling older, less financially viable skilled nursing and senior housing assets into dedicated behavioral health facilities. Yields range from about 8-9%, on par with skilled nursing cap rates.
“You really have to vet the opportunity,” said Feldman. Is there a market for acute inpatient psychiatry services? Will all the services offered be reimbursed by payers? Medicare has a strong base rate for mental health treatment. But, he warned, “Do your homework.”
Nevo-Hacohen added that the availability of capital is limited in the behavioral space. Few operators have a solid track record. Debt is scarce. Equity investors are focused on building platforms to roll up properties. “It’s a very fragmented space,” said Nevo-Hacohen, who added that Sabra is helping to fill the capital gap.
On the services side, hospitals are looking for alternative providers with mental health programs. Value-based care insurers recognize the need to house patients in the right level of care. Forman thinks this could be an opportunity for senior living providers if they have the right programming in place.
Senior housing operators don’t have to hire mental health professionals, the panelists agreed. “Think about how to affiliate with providers who can bring those services in,” said Feldman. Program discussions should include the entire treatment team, both internal and external. “Make sure everyone is on the same page,” said Forman.
Bringing the discussion full circle, Feldman emphasized the importance of integrating physical and mental health care. “Psychiatry is a medical issue,” he said. “It’s not distinct from treating heart failure, obesity, diabetes, or anything else.”