A look back at a year’s worth of data on COVID-19 case counts in U.S. nursing homes reveals some surprising insights, and some important questions. The data indicate that U.S. skilled nursing facilities (SNFs) are currently the safest places to be for frail older adults, who are most susceptible to the virus. In fact, case counts within SNFs are down 98% since the December 20th launch of the long-term care vaccination program. By May 16, they accounted for about 0.3% of U.S. cases.
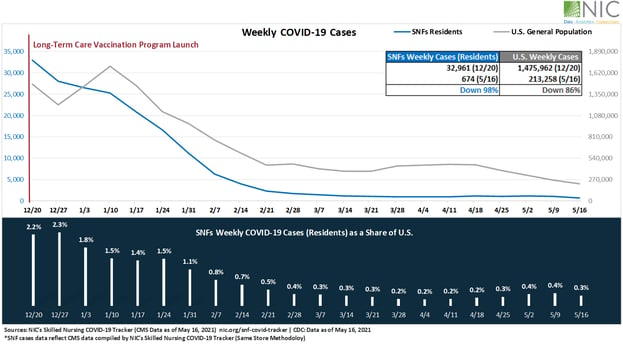
The drop in nursing home cases has outstripped the drop in case counts amongst surrounding populations, which in some areas were on the rise, even as vaccines become more readily available. In December 2020, new nursing home fatalities accounted for about 74% of overall fatalities for older adults over 85 years of age. By April 2021, that share dropped to 28%. Currently, more fatalities are occurring in the general population of older adults over 85 years of age than in those living in nursing homes.
At NIC, we’ve been analyzing and tracking Centers for Medicare and Medicaid (CMS) data throughout the pandemic, since March of last year. Our interactive “Skilled Nursing COVID-19 Tracker” (Tracker) tool is updated weekly with fresh CMS data. The tool can be used to compare weekly infections of COVID-19 in skilled nursing facilities, as well as in the U.S. general population, and can be geographically searched across regions, sub regions, and states.
Nursing Homes vs Local Populations
The data clearly tracks with the nationwide effort to prioritize nursing home residents for vaccinations. Case counts began to steeply decline as the Pfizer, and then the Moderna vaccines began to be distributed to nursing homes across the country on December 20, 2020. Nursing home case counts remain low, particularly when compared to infection rates among the general population, which have roared back in recent weeks.
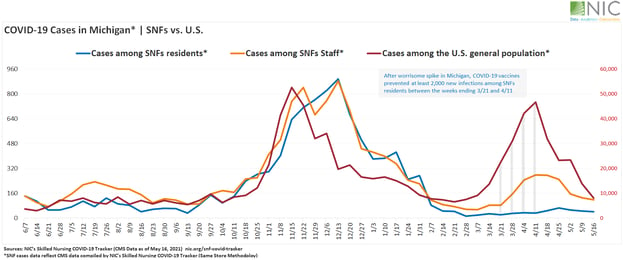
In the Midwest, over three months into the U.S. vaccination program, Michigan reported the highest statewide general population increase in COVID-19 cases, jumping 612% from February 21 to April 11, reaching highs not seen since vaccines first became available. The state’s case count among residents in SNFs, however, declined 25% over the same period. Meanwhile, cases among staff increased 281%. Between the weeks ending March 21 and April 11, COVID-19 vaccines prevented at least 2,000 new infections among SNFs residents in Michigan.
Overall, COVID-19 cases among residents dropped to lowest point in pandemic, only 6 in 10,000 nursing home residents tested positive for COVID-19 for the week ending May 16, which, compared to over 300 in 10,000 back on December 20, 2020, reflects the magnitude of the impact of the U.S. vaccination program on nursing home residents. Five months into the vaccination program, 42 states and geographies were reporting 20 cases or less across their entire nursing home populations.
The Risk of Unvaccinated Staff
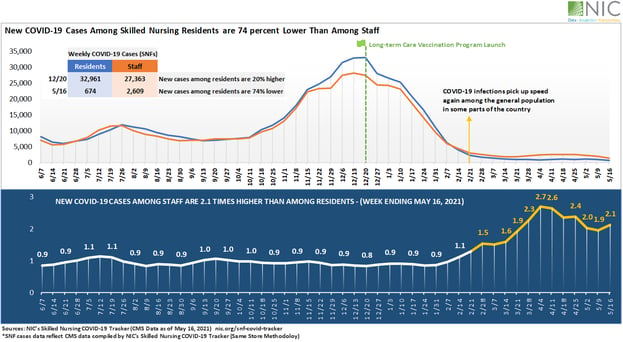
Tracking back one year, from this month to last May, Tracker data reveals that despite the swift and immense impact of vaccinations, a troubling risk persists. At the height of the pandemic, new cases among skilled nursing residents were 20% higher than among staff. However, the trend has reversed in recent weeks: newly confirmed cases among residents were 74% lower than among staff on May 16. We already know that, even with the proper safety protocols and equipment, this vector represents a grave risk to the nursing home community.
Other NIC data sources, such as the Executive Survey Insights (ESI), a bi-weekly survey of senior living operators, help to support and explain some of the patterns we can see in the Tracker data. Yielding data on properties of every size, type, ownership structure, and across each care segment, every completed ESI questionnaire delivers information from the perspective of an owner/operator’s entire portfolio of seniors housing and nursing care properties. The ESI has been providing real-time insights on hundreds of buildings and thousands of units across the country every two weeks since near the beginning of the pandemic.
Roughly nine out of ten respondents in the Wave 22 ESI survey indicated that educating and motivating staff to take the vaccine was a challenge. This data, though anecdotal, may help explain why Tracker data is now showing that COVID-19 cases amongst staff, though significantly lowered, are failing to keep pace with the drop in resident infection rates. Already struggling with staffing shortages and high turnover rates, and often resorting to hiring temp agency workers, some nursing home operators may be unable to achieve a 100% staff vaccination rate, even when they have access to vaccines. Given the risks once COVID-19, and its variants, enters any congregate living setting, this dynamic represents a persistent threat that vaccine availability alone cannot remedy.
Not All Nursing Homes Are the Same
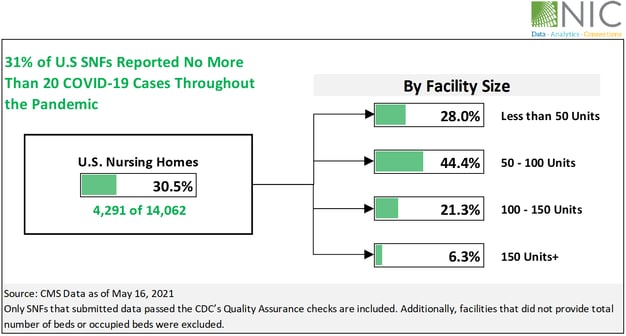
Tracking cases from the beginning of the pandemic to May 16, 2021, at which point nursing homes residents across the country were nearly universally vaccinated, it becomes clear that nursing home safety varies widely. In fact, nearly one third of U.S. nursing homes reported no more than 20 COVID-19 cases in total over that period, since CMS started reporting data. Sadly, fewer than 20 cases is a relatively low number. NIC looked more closely at this category of nursing home.
Data suggests that nursing home size may be a factor. Of all the nursing homes reporting fewer than 20 total cases throughout the pandemic, 44% were in the 50-100 unit size range. Six percent were in the largest category of 150+ unit facilities. Small nursing homes, with fewer than 50 units, performed slightly better, at 28% nationally, than those in the 100-150 unit size range, 21% of which reported fewer than 20 cases overall. The 50-100 unit size range outperformed the others.
Some nursing homes managed to completely block COVID-19 from infecting their residents. This was the case, even in geographic locations that saw significant community spread. Overall, about 4.5% of U.S. nursing homes reported 0 cases throughout the pandemic, from the time CMS began reporting data to May 16, 2021. This data indicates that there may be lessons to learn from those facilities, particularly as they kept out COVID-19 even before the vaccine was made available.
Questions on Safety
According to CMS pandemic data through May 16, 2021, 25% of nursing homes are responsible for 54% of total resident cases. The remaining 75% are responsible for only 46% of overall cases. For the largest properties of over 150 units, 80% of cases were reported by only 56% of communities.
Why did some nursing homes outperform others in keeping residents safe from COVID-19? Is there a ‘Goldilocks principle’ on the ideal size for a nursing home? Data suggests that communities of 50-100 units are safer than those that are bigger and smaller. But, as is so often the case, the data fails to provide all the answers. The questions that this data raises, however, may be the right ones to ask, as we work to ensure the safety of older adults, even as the pandemic continues.
About Beth Mace and Omar Zahraoui
Beth Burnham Mace is a special advisor to the National Investment Center for Seniors Housing & Care (NIC) focused exclusively on monitoring and reporting changes in capital markets impacting senior housing and care investments and operations. Mace served as Chief Economist and Director of Research and Analytics during her nine-year tenure on NIC’s leadership team. Before joining the NIC staff in 2014, Mace served on the NIC Board of Directors and chaired its Research Committee. She was also a director at AEW Capital Management and worked in the AEW Research Group for 17 years. Prior to joining AEW, Mace spent 10 years at Standard & Poor’s DRI/McGraw-Hill as director of its Regional Information Service. She also worked as a regional economist at Crocker Bank, and for the National Commission on Air Quality, the Brookings Institution, and Boston Edison. Mace is currently a member of the Institutional Real Estate Americas Editorial Advisory Board. In 2020, Mace was inducted into the McKnight’s Women of Distinction Hall of Honor. In 2014, she was appointed a fellow at the Homer Hoyt Institute and was awarded the title of a “Woman of Influence” in commercial real estate by Real Estate Forum Magazine and Globe Street. Mace earned an undergraduate degree from Mount Holyoke College and a master’s degree from the University of California. She also earned a Certified Business Economist™ designation from the National Association of Business Economists.
Omar Zahraoui, Principal at the National Investment Center for Seniors Housing & Care (NIC), is a seniors housing research professional with expertise in providing quantitative analysis and insights on seniors housing & care market data; building new products and reporting capabilities, including dashboards and proformas for clients and internal stakeholders; and implementing new processes and data solutions. Prior to his current role, Omar worked as a data analyst, at Calpine Corporation, supporting the development of new-business strategy initiatives, analyzing sales and financial data, and developing statistical modeling of consumers’ behaviors to drive business performance. Omar holds a Bachelor’s degree in Business Administration with concentrations in Finance and Management, a Master in Corporate Finance from IAE Lyon School of Management at Jean Moulin Lyon III University in France, and a Master of Science in Management Information Systems and Data Analytics from Pace University.
Connect with Beth Mace and Omar Zahraoui
Read More by Beth Mace and Omar Zahraoui